Breastfeeding
Breastfeeding has multiple benefits, including reduced risk of gastrointestinal problems and respiratory infections. UK breastfeeding rates lag behind comparable high income countries.
This indicator was published in March 2020.
In May 2021 we updated our graphs and charts where new data had been published, and we reviewed our policy recommendations by nation.
Background
- Breastfeeding is part of the natural reproductive process. It has significant and lifelong benefits for both mother and child, including a reduced risk of gastro-intestinal problems, respiratory infections, lower rates of hospital admissions for babies, and protection against breast cancer for mothers.1 There is growing evidence that breastfeeding protects against the risk of respiratory tract infections in childhood2 and becoming overweight or obese throughout the life course.3
- Breastfeeding initiation rates in the United Kingdom are lower than in many comparable high-income countries4 and have shown minimal improvement in recent years.
- Breastfeeding rates are reported as mixed (partially breastfeeding) or exclusive breastfeeding (infants only receiving breastmilk). Across the UK, the way in which rates are reported, and the denominators used, vary slightly across the four nations, so care should be taken in comparisons between nations.
Key findings
- Since 2015/16, a small yearly increase has been observed in rates of breastfeeding: both exclusive and partial breastfeeding in Scotland (at 6-8 week review)5; Northern Ireland (at 6-8 week review)6 and Wales (at 6 week review).7
- This pattern was mirrored in England until 2017/18, however the latest data shows a slight decline in rates of exclusive breastfeeding at 6-8 week review, with 42.7% of mothers breastfeeding (either exclusively or partially), the lowest proportion since 2009/10.8
- Mothers in the most deprived areas have consistently lower rates of initiating and continuing breastfeeding compared to those in the least deprived, in England and Wales,9 Scotland5 and Northern Ireland.6
Breastfeeding status is collected at 6 weeks in Wales and at 6-8 weeks in England, Northern Ireland and Scotland.
What does good look like?
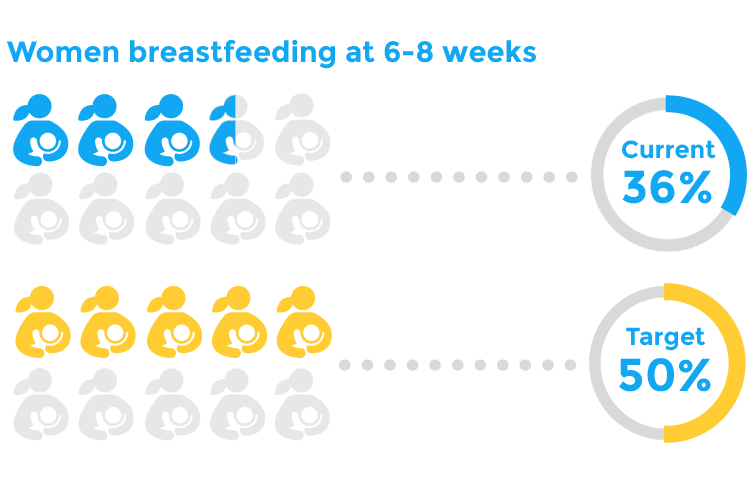
Meet Government targets to increase rates of initiation and continuation of breastfeeding. The UK government recommends exclusive breastfeeding for around the first 6 months of life,10 which supports the World Health Organisation’s global nutrition target to increase exclusive breastfeeding rates in the first 6 months to at least 50%.11 Latest available data from 2010 shows that only 34% of women in the UK were still breastfeeding their babies by six months, and only 1% were exclusively doing so.7 The percentage of babies who are not breastfed (or have an unknown feeding status) at 6 to 8-week review in England, Scotland and Wales ranges between 56-71% (at 2015/16).8,5,7
Provide greater support and education to sensitively promote the benefits of breastfeeding and the normalisation of breastfeeding. A multi-disciplinary approach to delivering breastfeeding advice and evidence-based support will help mothers to make informed choices about breastfeeding, and foster a broader culture that encourages ongoing breastfeeding. A survey conducted by Public Health England in 2016 highlighted themes around uncertainty with how to breastfeed, what to consider when breastfeeding, and embarrassment around breastfeeding in public as potential barriers.12 Communication campaigns to help address uncertainties and educate mothers are necessary as well as offering peer-to-peer and group support schemes, especially to reduce inequalities between groups. At the same time, mothers who cannot, or choose not to, breastfeed should be respected with support and infant feeding education provided.
Services who care for babies and their mothers to achieve Baby Friendly Accreditation status. This status signals that healthcare services are designed to promote the needs of babies and their parents, and is supported by evidence-based standards to improve both the numbers of babies receiving breastmilk and exclusivity of breastfeeding.13
Strengthen and standardise data collection on breastfeeding across all four nations to ensure the availability of reliable, comparable data and the continued monitoring of trends.
I would just tell people it's natural and normal
Policy recommendations
- Department of Health and Social Care should conduct an Infant Feeding Survey, to ensure that there is improved data collection on rates of breastfeeding continuation at birth, 10-14 days, 6-8 weeks, and 6 months. We welcome the commitment within the Department for Health and Social Care’s Prevention Green Paper to support this.
- All Integrated Care Systems (ICS) should develop local plans for breastfeeding, in collaboration with Local Maternity Action Boards. This should include monitoring local breastfeeding data.
- UK Government should resource Local Authorities to provide local pathways, agreed by multi-agencies, which improve access to support, resources and services for women seeking to breastfeed. These pathways should include provision of local breastfeeding peer support networks.
- Funding for these services should be ringfenced within areas with high maternal deprivation.
- Department of Health and Social Care should deliver a public health messaging campaign on initiation and continuation of breastfeeding. Campaigns should be targeted in areas with high maternal deprivation.
- Scottish Government should repeat the Scottish Maternal and Infant Nutrition (2017) survey on a biannual basis and include data collection on rates of breastfeeding at birth, 10-14 days, 6-8 weeks, and 6 months.
- Local Authorities should provide local pathways, agreed by multi-agencies, which improve access to support, resources and services for women seeking to breastfeed. These pathways should include provision of local breastfeeding peer support networks. Funding for these services should be ringfenced within areas with high maternal deprivation.
- Public Health Scotland should deliver an evidence-based approach to communications around breastfeeding designed to bring about social change and normalise breastfeeding in Scotland. Scottish Government should provide additional funding for this campaign, which should be targeted in areas with high maternal deprivation and broadcast through print and digital media.
- We welcomed the Welsh Government’s launch of the All Wales Breastfeeding Five Year Action Plan in 2019. Resource should be provided to ensure implementation of actions within the Plan.
- We welcome local action plans for all Health Boards to support implementation, including actions for local peer support networks and an infant feeding lead for each Health Board.
- In 2020, Welsh Government should support the national steering group to oversee delivery and ensure monitoring of the Action Plan.
- The Action Plan should ensure improved data collection on breastfeeding rates; including the Plan’s own recommendations for data collection at birth, 10-14 days, 6-8 weeks and 6 months.
- Welsh Government and Public Health Wales should deliver an evidence-based approach to communications around breastfeeding designed to bring about social change and normalise breastfeeding in Wales. Public health messaging campaigns should be targeted in areas with high maternal deprivation.
- We welcome that all hospitals providing maternity services in Northern Ireland are now accredited as “Baby Friendly” under the WHO/UNICEF Baby Friendly Initiative, as are four of five HSC Trust health visiting services. All five Trusts should attain this accreditation.
- We welcome that the Northern HSC Trust maternity and health visiting services achieved the first joint UK “Baby Friendly” Initiative Gold Standard, the remaining Trusts should work toward achieving this standard.
- HSC Trusts should provide access to peer support networks as well as trained counsellors across Northern Ireland and funding for these services should be ringfenced within areas with high maternal deprivation.
- We welcome the #NotSorryMums breastfeeding campaign. The Public Health Agency should provide recurrent funding for this campaign on initiation and continuation of breastfeeding. Future campaigns should be targeted in areas with high maternal deprivation.
- The Department of Health should introduce legislation to support and protect breastfeeding infants and their mothers in public places.
What can health professionals do about this?
- Breastfeeding advice. All child health professionals should be trained to deliver simple breastfeeding advice. They should make it their responsibility to be aware of specialist advice and local services to support breastfeeding, in order to signpost mothers effectively.
- Make every contact count. Mothers may see any encounter with a trusted health professional as an opportunity to discuss breastfeeding. Professionals should take the opportunity to proactively explore and promote breastfeeding practices, in a sensitive manner.
- Maintain a respectful approach. If a woman chooses not to breastfeed after being given appropriate information, advice and support,her choice must be respected by healthcare professionals.14
Contributing authors
- Dr Ronny Cheung, RCPCH State of Child Health Clinical Lead
- Karina Green, RCPCH Research & Quality Improvement Division
- Rachael McKeown, RCPCH State of Child Health Project Manager
- Dr Rakhee Shah, RCPCH State of Child Health Clinical Advisor
Royal College of Paediatrics and Child Health (2020) State of Child Health. London: RCPCH. [Available at: stateofchildhealth.rcpch.ac.uk]
References
Victora, C. et al. 2016. Breastfeeding in the 21st century epidemiology, mechanisms, and lifelong effect. The Lancet.
The Lancet. Web appendix 4: Lancet breastfeeding series paper 1. data sources and estimates: countries without standardized surveys. 2016.
Victoria CG, Bahl R, Barros AJD, et al, for The Lancet Breastfeeding Series Group. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet 2016; 387: 457-90
UNICEF. 2018. Breastfeeding: A Mother’s Gift, for Every Child. New York: United Nations Children’s Fund.
Information Services Division. 2018. Infant Feeding Statistics Scotland: Financial Year of Birth 2017/18. National Statistics.
Public Health Agency. 2018. Health Intelligence briefing: Breastfeeding in Northern Ireland, September 2018.
Welsh Government. Stats Wales. Breastfeeding.
Public Health England. 2019. Official Statistics: Breastfeeding prevalence at 6-8 weeks after birth (experimental statistics). London: Public Health England.
NHS Digital. 2012. Infant Feeding Survey – UK, 2010.
Public Health England. 2019. Breastfeeding and dental health.
World Health Organization. 2014. Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition. Switzerland: World Health Organization.
Public Health England. 2017. Press Release: New survey of mums reveals perceived barriers to breastfeeding.
UNICEF. Date unavailable. Baby Friendly Initiative.
Royal College of Midwives. 2018. Position Statement on Infant Feeding. London: royal College of Midwives.
