Prevalence of mental health conditions
Half of mental health conditions in adults start before the age of 14 and 75% before the age of 24. Prevalence of all types of mental health conditions are increasing in England.
This indicator was published in March 2020.
In May 2021 we updated our graphs and charts where new data had been published, and we reviewed our policy recommendations by nation.
Background
- Mental health is a public health priority that requires actions and investment to promote wellbeing in children and young people. Three quarters of life-long mental health problems in the UK start before the age of 25 and today’s children and young people are considered to have worse mental health outcomes compared to previous generations.
- There are limited objective data on the prevalence of mental health disorders among children and young people across all of the UK nations, and what data there are usually rely on self-reported indicators of wellbeing or life satisfaction. This indicator analyses data available from the Mental Health of Children and Young People’s Survey of England,1 which provides more detailed information on the types of mental health disorders children and young people have.
- Mental health problems are commonly classified into four major groups:
- Emotional disorders (such as anxiety disorders, depressive disorders, mania and bipolar affective disorder)
- Behavioural disorders (characterised by repetitive and persistent patterns of disruptive and violent behaviour, in which the rights of others, and social norms, are violated)
- Hyperactivity disorders (characterised by inattention, impulsivity, and hyperactivity)
- Others (such as autistic spectrum disorder, tic disorders or eating disorders).
I think it’s equally important, it might even be more important than physical health.
Key findings
- Detailed data are reported here only for England (based on the Mental Health of Children and Young People’s Survey), as detailed recent data on mental health problems (rather than wellbeing) were not available for the other countries.
- From 1999 to 2017, prevalence of all mental health disorders among children aged 5-15 rose slightly (1.5 percentage point) from 9.7% to 11.2%.
- Mental health disorders were more common, and rose more dramatically, in older children. Prevalence was 13.6% of children aged 11-15, compared with 9.5% aged 5-10 in 2017 – and while both age groups showed an increase over time, it rose more for the older age group.
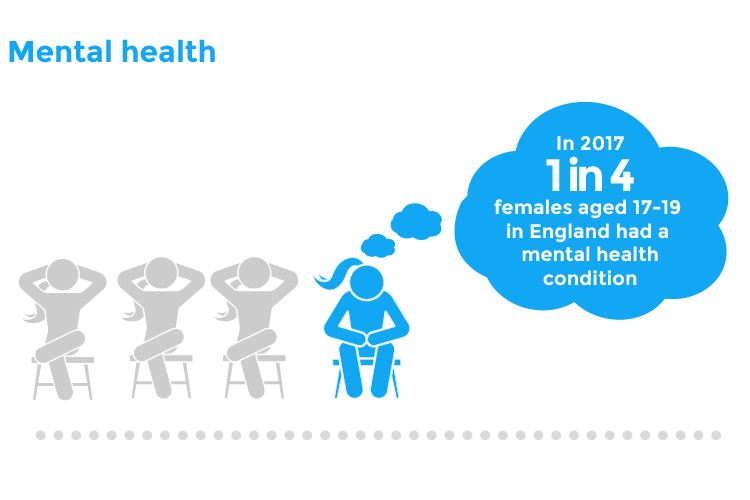
- One in six (16.9%) young people aged 17-19 had a mental health disorder in 2017.
- The sharpest prevalence rise for children aged 5-15 has been within emotional disorders (for example: anxiety, depression, OCD, phobias), increasing from 4.3% to 5.8% from 1999 to 2017. Slightly more girls than boys suffered from emotional disorders in 2017 (6.1% compared to 5.6%), although the increasing trend is seen for both genders. 14.9% of young people aged 17-19 have emotional disorders in 2017, rising to 22.4% of women for this age group.
- Prevalence of behavioural disorders and hyperactivity disorders in children aged 5-15 have remained largely stable
- Behavioural disorders prevalence fell only by 0.7 percentage points between 2004 and 2017, and in fact has been largely unchanged since 1999. Behavioural disorders are more common in boys than girls, 7.1% compared to 3.9% in 2017.
- Hyperactivity disorders prevalence has remained relatively stable from 1999 to 2017 and are more common in boys. The total percentage is relatively low (1.9% of children aged 5-15 in 2017) in comparison with the other mental health disorders.
No comparable mental health prevalence data is available for Northern Ireland, Scotland or Wales.
What does good look like?
Increased data collection on the prevalence of mental health problems in children and young people. To better understand the level of need for mental health services, we require routine data collection across the UK. The recent NCEPOD report on quality of care for children and young people admitted to hospital for mental health problems concluded that there are huge variations in quality, definitions, accessibility of national data relating to mental health.2 Furthermore, children not being seen within a dedicated mental health service are not recorded and are essentially ‘missing’ from the data.
Policy recommendations
- We welcome the 2020 Mental Health of Children and Young People in England Survey. NHS Digital should conduct this survey a minimum of every three years to improve data collection on children and young people’s mental health, enabling greater recognition of the level of need.
- Scottish Government should introduce and fully fund criteria free, community-based therapies for all children and young people, as well as family therapy to address all levels of mental health needs.
- Local Authorities should provide local pathways, agreed by multi-agencies, which improve access to support, resources and mental health services.
- Scottish Government should collect data on the prevalence of mental health conditions in children and young people and report this at a minimum of every three years.
- Welsh Government should continue to resource Time to Change Wales, which provides a national campaign to reduce stigma of mental health problems (delivered by Mind Cymru and Hafal).
- Welsh Government should collect data on prevalence of mental health conditions in children and young people and report this at a minimum of every three years.
- Northern Ireland should improve data collection on children and young people’s mental health. We welcome the transformation funding which was allocated to the HSC Board to conduct a prevalence study which is currently underway and due to complete in 2020 – this should be repeated a minimum of every three years.
What can health professionals do about this?
- Early recognition and identification of need. Health professionals must be alert to signs and symptoms of mental as well physical ill health, in order to signpost or refer onto appropriate services for support or treatment in a timely manner. This includes being aware of the biopsychosocial model of disease, and a recognition that psychological problems often manifest with physical symptoms.
- Improved mental health training for health professionals. Mental health should be a core part of the training curriculum for all health professionals who deal with children and young people. One useful resource is the e-learning provided through the MindEd resource which helps professionals identify and help children and young people with mental health issues. There are modules designed for families too, to which professionals may wish to signpost carers.
- Advocate for the mental health of local children and young people. Use available data on mental health prevalence and service capacity to articulate the needs of your local population, to advocate for adequate provision of mental health services to local decision makers, from NHS commissioners, to social care, education and local government.
- Encourage integrated working between organisations and agencies across the whole children’s workforce. Integration of practice, education, pathways and commissioning will ensure that prevention, recognition, early intervention, support and onward referral is commonly addressed by professionals.
Contributing authors
- Dr Ronny Cheung, RCPCH State of Child Health Clinical Lead
- Rachael McKeown, RCPCH State of Child Health Project Manager
- Dr Rakhee Shah, RCPCH State of Child Health Clinical Advisor
Royal College of Paediatrics and Child Health (2020) State of Child Health. London: RCPCH. [Available at: stateofchildhealth.rcpch.ac.uk]
References
NHS Digital. 2018. Mental Health of Children and Young People in England, 2017 [PAS].
Healthcare Quality Improvement Partnership (2019). Mental Healthcare in Young People and Young Adults.
