Conceptions in young people
Teenage pregnancy is associated with poor outcomes for young women and their children. Encouragingly, conception rates among 15-17 year olds are decreasing across the UK.
This indicator was published in March 2020.
In May 2021 we updated our graphs and charts where new data had been published, and we reviewed our policy recommendations by nation.
Background
- Teenage pregnancy is associated with poor outcomes for young women and their children. For mothers, there is a higher risk of poor educational attainment, social isolation and poorer mental and physical health, while their children are more likely to be born preterm or with low birthweight.1
- While not all teenage conceptions are unplanned, teenagers remain at highest risk of unplanned pregnancy, with over 50% of under-18 conceptions in England and Wales in 2017 ending in abortion.2
- There are individual and social risk factors for teenage pregnancy, including: adverse childhood experiences; socioeconomic deprivation; attention, behaviour and conduct problems; poor educational attainment and engagement; and family history of teenage pregnancy.3
- Reducing teenage pregnancy requires comprehensive relationships and sex education and access to effective contraception in youth friendly services. Dedicated coordinated support for young parents helps improve outcomes for them and their children.4
- This indicator examines conceptions, which includes those ending in livebirth, stillbirths and where the pregnancy was terminated. Comparable data are not available for Northern Ireland, whose legislation differs from the rest of the UK in deeming termination of pregnancy illegal except where the health of the woman is at risk.
Key findings
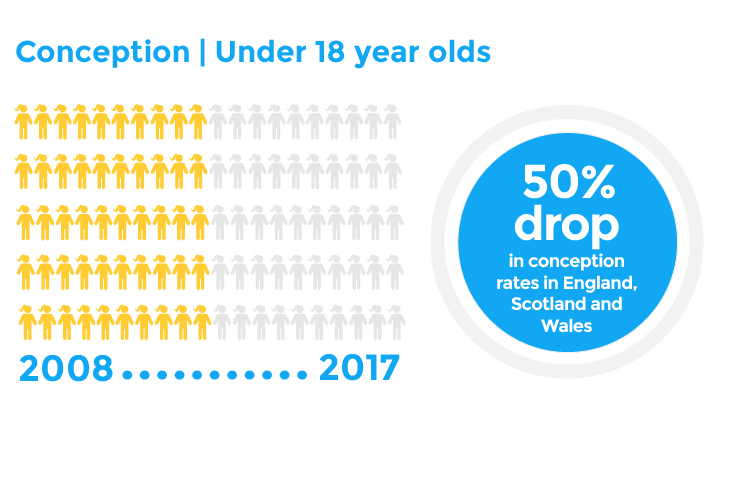
- The last ten years have seen a sustained decline in conception rates for 15- to 17-year-old females across England, Scotland and Wales. From 2008, conceptions per 1,000 have significantly reduced, with declines reported in England of 39.7 to 17.3 (2018), Scotland 40.0 to 16.3 (2017) and Wales 43.7 to 19.5 (2018).
- Conception data for Northern Ireland are not available, which relates to the data limitations associated with the differences in legislation around termination of pregnancy compared to the rest of the UK. Live birth rates for 15- to 17-year-old females show a declining trend from 10.5 births per 1,000 in 2008 to 4.7 in 2017.
- Under-18 conception rates remain considerably higher amongst young women living in the most deprived areas, although there have been reductions across all deprivation subgroups between 2014 and 2016.
What does good look like?
Reach comparable conception rates with similar European countries. While the UK continues to see a steady decline in the under-18 birth rate over the past two decades, the rate remains much higher than many similar comparable, western European countries, with the latest comparisons ranking the UK 22nd out of 28 EU countries. In 2015, the UK recorded 6.4 births per 1,000 for women aged 15-17 whereas the lowest rates in Europe are recorded in Denmark (0.8 per 1,000), the Netherlands (1.1 per 1,000) and Switzerland (1.5 per 1,000). In comparison to these countries, the UK still has considerable opportunity to improve and should aim to learn from successful interventions in these lowest rate countries.5
Universal access to reproductive and sexual health education is critical to maintaining progress on reducing teenage pregnancy and improving sexual health. The introduction of universal Relationships education, relationships and sex education (RSE) and health education curriculum in English schools from 2020 is a welcome opportunity to embed universal primary prevention on health messages for all children and young people.6
Target interventions for young women in living in high risk or deprived areas. There is significant geographical variation in rates of teenage conception, and the declines seen across the under-18 conception rate is not equal when broken down across socioeconomic group.7 Based on 2016 data from Scotland, significantly higher rates of conception are seen in the most deprived quintile (36.4 conceptions per 1,000 females) compared to the least deprived (6.6 per 1,000). While reproductive and sexual health education, and contraception services, should be universally offered, those living in deprived areas are at greater risk and require additional support.
Policy recommendations
- UK Government should provide more funding for Local Authorities to expand and deliver sexual health services.
- Scottish Government should provide extra funding for Local Authorities to expand and deliver sexual health services.
- Welsh Government should provide extra funding for Local Authorities to expand and deliver sexual health services.
- The Department of Education should ensure that the full complement of relationships and sexuality education (RSE) as set out by the reviewed CCEA guidance is delivered to all pupils across Northern Ireland, to ensure that consistent and meaningful education is delivered to all young people. The quality of this education should be inspected by the Education Training Inspectorate.
What can health professionals do about this?
- Signpost young people to local sexual health services for reproductive and contraception advice and contraceptive services.
- Support pregnant young women to access healthcare. Young women who are pregnant often find accessing healthcare, especially antenatal care, challenging. NICE guidance suggests that young women should be supported by professionals:
- offering age-appropriate services
- being aware that the young woman may be dealing with other social problems
- offering information about help with transportation to and from appointments
- offering antenatal care for young women in the community
- providing opportunities for the partner/father of the baby to be involved in the young woman’s antenatal care, with her agreement.8
These principles could apply equally to antenatal and to family planning or contraception clinics.
- Make every contact count. Use clinical consultations as an opportunity to sensitively explore whether young people are having difficulty with relationship or sexual health concerns, where appropriate. RCPCH’s Young People’s Special Interest Group recommends using the HEADSSS assessment framework to explore pertinent psychosocial issues with young people.
- Resources for practitioners and service planners:
Contributing authors
- Dr Ronny Cheung, RCPCH State of Child Health Clinical Lead
- Rachael McKeown, RCPCH State of Child Health Project Manager
- Dr Anna Rossiter, RCPCH Research & Quality Improvement Division
- Dr Rakhee Shah, RCPCH State of Child Health Clinical Advisor
Royal College of Paediatrics and Child Health (2020) State of Child Health. London: RCPCH. [Available at: stateofchildhealth.rcpch.ac.uk]
References
Hoffman SD, Maynard R. (2008) Kids Having Kids: Economic Costs & Social Consequences of Teen Pregnancy. Washington, DC: The Urban Institute Press, USA.
ONS (2019). Conceptions in England and Wales: 2017. Available from ONS.
Woodward L, Fergusson DM, Horwood LJ. (2001). Risk factors and life processes associated with teenage pregnancy: Results of a prospective study from birth to 20 years. J Marriage Fam. 63:1170–84
Hadley, A, Ingham, R and Venkatraman C-M. (2018) Teenage Pregnancy and Young Parenthood: effective policy and practice. Routledge
Office for National Statistics. 2017. Live births to women aged “Under 18” and “under 20”, (per 1,000 women aged 15 to 17 and 15 to 19) in EU28 countries, 2005, 2014 and 2015. Available from ONS.
DfE (2019). Relationships education, relationships and sex education (RSE) and health education. Available from UK Gov.
Office for National Statistics. 2014. Teenage conception rates highest in the most deprived areas. Short story published in Conceptions-Deprivation Analysis Toolkit.
NICE (2010) CG110. Pregnancy and complex social factors: a model for service provision for pregnant women with complex social factors. Available from NICE.
Public Health England (2019). Teenage Pregnancy Prevention Framework. Available from UK Gov.
Public Health England (2019). A Framework to support teenage mothers and young fathers. Available from UK Gov.
